I was very pleased to be asked to come to talk to you today about Natural Birth after Caesarean, as this is an issue of extreme importance to a growing number of women. I am pleased that we have now reached a point where the term VBAC, vaginal birth after caesarean, is in common usage and I intend to use that term throughout this presentation.
To begin, I think I need to say a little about myself and how I have come to be standing here today, and why, despite some nerves, I am keen to make the most of this opportunity to talk to you.
My experience of caesareans began over 20 years ago with the birth of my daughter, followed 20 months later by the birth of my son, both born by caesarean section. I had a need for more information in order to try to understand what had happened to me and to try to come to terms with the experience. I soon found myself sharing this information and providing support to other women, at first locally, then nationally and recently internationally.
I teamed up with another caesarean mother, Gina Lowdon with whom I have worked closely with ever since. We took on a national role within NCT about 13 years ago.
One of our early tasks was to update the NCT's 8 page caesarean information leaflet - we eventually condensed our draft to just over 60 pages which make up the first edition of the NCT book "Caesarean Birth - Your Questions Answered"; this was published in 1996 and the second, slightly longer, edition followed in 2004.
In May 2002 we launched the website www.caesarean.org.uk, the site is intended to provide information about all aspects of caesarean birth. The last 5 years has seen much of the telephone support that we used to provide move to email; fortunate timing for us, as we have both returned to paid work and we can now answer these enquiries at unsocial hours that would not have been possible with telephone enquiries. We feel that the site has struck a good balance and we continue to receive emails from women wanting to avoid caesareans and others wanting to arrange one.
I have been privileged to talk to literally thousands of women about their experiences of caesareans and VBAC; they are the ones that have given me the insights that I want to share with you today.
I would like you to take a moment to think about the discussion you might have in your role as a health professional with a woman who has had a previous caesarean and who is now pregnant again. What information do you think that she needs to be given about her next birth? And what would you want to know about her previous birth? How would information about the previous birth impact your discussion?
I want to try to give you an insight into the woman's perspective of the information she may receive from you, and consider why the information that many women receive from the health professionals may not be ideal for a woman considering VBAC.
For most women planning or considering a VBAC their only experience of birth will be one that ended in a caesarean. They are now in the position of planning for a birth that they intend to end differently to the previous experience. So their focus will obviously be on how this birth is going to be different to the last one, how they can make it different, what they can do to avoid repeating the previous experience.
For the women that had a caesarean for placenta previa, twins or because their baby was breech - the crucial points will come when the placenta is not this time near the cervix, a single baby is confirmed or the baby is head down. Once they pass this hurdle they are back as they would have been in a first pregnancy, in the unknown, needing the support that any first time mother would need, but not struggling to find a way to avoid the previous experience. It is interesting that studies show that this is the group of women who achieve the highest rates of vaginal birth in subsequent pregnancies.
However, the largest group of women will have had caesareans because their labour had not progressed quickly enough or because their baby became distressed. Some women will have just accepted this as bad luck and will be able to try again without too much reference to the previous experience. However, I suspect that they are the minority. Even women I have spoken to who profess to be at peace with their caesarean for failure progress, or fetal distress rarely seem to be quite so content if you are prepared to listen fully to their experience. We don't have to prompt them, just listen in a non-judgemental way for a short while and many of these women will open up and reveal a whole host of concerns about the way they were supported and their previous birth managed.
Many women will have put considerable mental effort into trying to understand why the previous birth did not proceed normally, for some it will have dominated every waking hour since the caesarean.

The majority of women in this situation will have identify for themselves reasons that they believe caused them problems, interventions during labour, " lack of support in labour, " an environment where they were not physically or psychologically comfortable are often referred to, but also " the journey to hospital, " unkind words, " pain relief offered rather than support - I could go on.
They often struggle to understand how these things could have affected the physical process of labour and birth. Their gut feeling is that these were the causes of their problems, but they do not have a mechanism to connect them. Information about the hormonal link between oxytocin driving labour and adrenaline suppressing it will often be a huge relief to them - they are finally able to put together the pieces of the jigsaw and make sense of their body's reactions.
There is often a huge relief that their body did not fail them, it worked beautifully, even if it misunderstood the situation. Take for instance the women whose labour slowed or stopped on arrival at hospital. Being able to understand that her body was reacting to the strange and unknown environment and people, and that consequently labour stopped or slowed so the birth would not happen until she had settled in and felt safe, can help women to trust their bodies again, something they will need to do if they are planning a VBAC.
So the logical conclusion will be to plan for a birth where the previous interventions and situations are avoided unless really necessary, to find good support for labour (and here the first choice of most women will be a known and trusted midwife) and to choose a place of birth that feels safe and secure.
So, what happens for these women when planning a VBAC; women whose previous experience was an unplanned caesarean during labour, women whose thoughts and feelings about this birth are likely to be dominated by their thoughts and feelings about the previous birth.
It seems that women are almost always given information first and foremost about the risk of rupture involved with a VBAC. They may be told that they can or can't have a VBAC based on their obstetric history; They may be told that they have a high/low chance of a successful VBAC based on the reason for the previous caesarean. And sometimes they are given a list of conditions that will be placed on during labour. However, often this list of conditions does not become apparent until late in pregnancy or when they are in labour.
The conditions placed on labour after a previous caesarean are often just those aspects of labour management that women feel they need to avoid in order to achieve a VBAC.
This seems to me to create a huge gap between what women need and what the majority of NHS services are offering them.
Where do VBAC women really stand? What are their rights?
I think that there is a general confusion about the status of VBAC. There seems to be the idea that VBAC is some form of treatment or intervention, something that a woman can be offered or denied. This is not the case; it is the repeat caesarean that is the intervention.
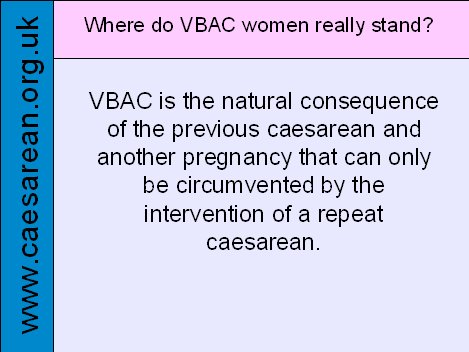
VBAC is the natural consequence of a previous caesarean and another pregnancy that can only be circumvented by the intervention of a repeat caesarean. If you think about it, it is ludicrous that a pregnant woman should feel she has to have someone else's permission to labour!
It is about time that all health professionals were honest to women about where they stand. " women should be offered the option of a repeat caesarean, " they should be offered the option of a hospital birth, " they should be offered the option of continuous monitoring;
but none of these are compulsory, these are all options that can be rejected or declined by women. In order to allow a woman to consent she must be allowed to make an informed choice. This does not mean she has to choose what her health professional considers the safest option, it does not even mean that she has to choose what she feels is the safest option, it means that she can consider how the risks and benefits impact her, and choose what she feels is right for her in the circumstances. Informed choice cannot be valid unless informed refusal is equally respected.
Not all women will want to take responsibility for decisions in this way, and some will want their health professional to advise them. Handing responsibility for a decision to someone else is making an informed decision too, but it is important that women are still given balanced information.
In order to make an informed choice about whether to accept the option being offered the women must have access to information about the risks and benefits of any proposed intervention - not all women will want these details, but many will, and without this information, or even worse, if misinformation is given, any consent obtained becomes very questionable.
In this country women have the right to maternity care, and the right to refuse any intervention or form of care, including admitting themselves to hospital, or having surgery - hence the option of a VBAC is always open to a women, even if it would be clearly dangerous for her or her baby. So is the option of HBAC (homebirth after a caesarean). Not that I am suggesting here that women will put their babies at unnecessary risk, just that they have the absolute right to make these decision for themselves, and to go against any medical advice. Medical professionals need to be more aware of women's right to autonomy.
So having established that VBAC women do not need anyone's permission to labour and do not have to accept any restrictions or conditions on their labours - what care should be offered to VBAC women?
There has been acknowledgement for at least 2 decades of the minimal additional risk that is involved with VBAC compared to other vaginal births.
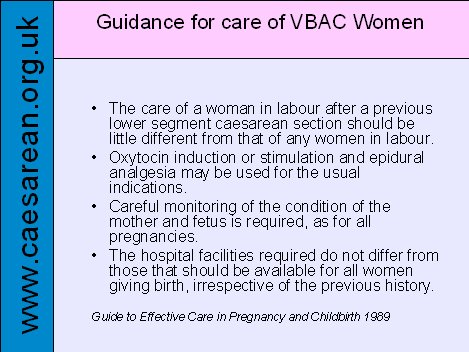
The Guide to effective care has been saying since 1989 that
Yet VBAC women are often treated as a situation waiting to go wrong. Yes, rupture is a serious problem, but it is not the only serious problem that a woman and her baby could encounter during a VBAC. If the chance of a rupture is compared with the chance of other serious problems, cord prolapse, placental abruption, etc. which also can be life threatening for the mother and the baby, then the overall risk of a serious problem is not significantly increased for a woman having a VBAC. So, I would encourage you to put this into perspective; a woman is more likely to have a real emergency caesarean, urgency category 1, which according to the caesarean section audit carried out in the UK in 2000, happens in about 2% of births, than to have one for a rupture which happens in half a percent or less of births.
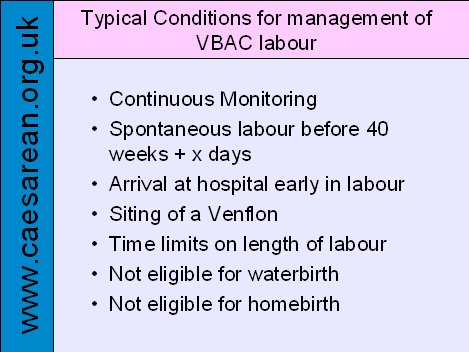
Let's now return to the sorts of conditions that women are frequently expected to comply with when planning a VBAC. Continuous monitoring, spontaneous labour before a certain number of days beyond 40 weeks, arrival at hospital early in labour, siting of a Venflon, time limits on each stage of labour, not eligible for waterbirth, not eligible for homebirth, etc.
Most women will accept these conditions because they are lead to believe that they increase safety. Despite that many women will find the conditions distressing, being sure that it was such practices that adversely affected their previous birth. For some the prospect of such conditions will lead them to rejecting VBAC altogether and wanting a repeat caesarean, whilst others will go ahead with their VBAC plans and will struggle to come to terms with the conditions imposed on them, and wonder how they are going to cope with labouring under such restrictions.
In the light of womens' concerns about how their labour will be handled, and their wishes to avoid the interventions that they associate with previous failure, and the pressure that is often asserted on them to accept these interventions; it is shocking for these women when they realise that such conditions are not based on research evidence. I want to consider the first two of these interventions in detail.
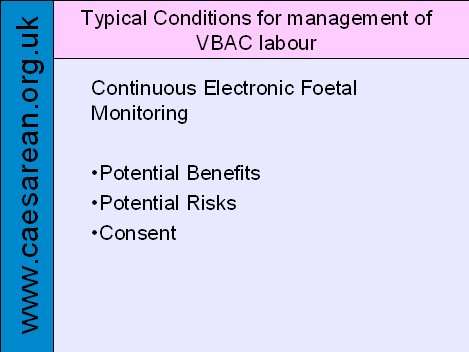
Continuous Monitoring - It seems that women having a VBAC are put under extreme pressure to accept continuous monitoring. It seems that many health professional find CFM reassuring, it is as though they can relax their observations of a women if the machine is there.
Women, however, find it restricts their mobility, something that can be very difficult when trying to labour effectively and instead of finding the machine reassuring, find it is a reminder of the fears of others; this has a psychological impact for the women, increasing her stress levels and leading via her hormones to adverse effects on her labour.
It is now clear that the benefits of continuous monitoring are limited to say the least. Although it is clear that fetal distress follows rupture there is no evidence that CFM will be any more effective at detecting this than intermittent monitoring. There are also many well respected health professionals who advocate watching for early signs of a problem, such as monitoring the woman's pulse and consider these an important aspect of safeguarding a VBAC mother and baby.
So, the benefits of CFM over intermittent monitoring are questionable at best, but what of the risks? It is very clear is that CFM leads to a significant rise in the number of unnecessary caesareans, with all the risks of an emergency repeat caesarean, including long term risks to the woman and risks during any subsequent pregnancy and to future babies. Making an estimate based on the figures from the latest Cochrane review on CFM, somewhere between 2% and 9% of VBAC women who are continuously monitored will have an unnecessary repeat caesarean in labour, just because they were monitored continuously. Avoiding continuous monitoring increases the success rate for VBAC and avoids some unnecessary emergency caesareans, with all the risks that these bring.
The NICE caesarean guideline recommends that women should be offered CFM during VBAC - if you follow the trail back this is based on information from the Electronic Fetal Monitoring guideline produced by RCOG and adopted by NICE, and this in turn is based on information from the 5th CESDI report, information which also recommends watching for other warning signs, but not only research evidence showing its effectiveness.

The EFM Guideline give a rate of dehiscence, acknowledges that these can present with a variety of warning signs, and that 'attentive intrapartum fetal and maternal surveillance in a setting where the baby can be delivered within 30 minutes' - it says nothing about CFM.
For a woman to be able to make a decision about whether to have CFM or to be able to give consent for continuous monitoring, she must be provided with information about the potential risks as well as the potential benefits, and to know that she will still be fully supported with her VBAC, should she decline the offer of CFM.
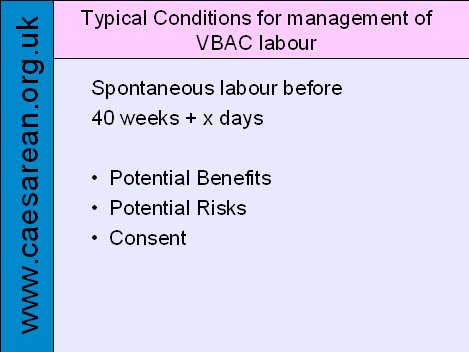
Spontaneous labour before 40 weeks + x days - Many women are being told that to be 'eligible' for VBAC they must go into labour by some specified time. Often this is 40 weeks and 10 days, but it is seems that some women are being expected to produce their VBAC baby at or before 40 weeks.
It seems that many are being told that they have two options. One is to be induced with the associated increased risk of rupture, and the other is to have a repeat caesarean - the option of waiting for labour is not even discussed. Waiting for labour to happen at 42, 43, or even 44 weeks must be an option for women, if they are to give proper consent for the alternatives. When this option is denied, the consent that they have given will have been given under duress and is of questionable legal status.
Women often contact us about how they are going to get labour going before some deadline that they have been given, they are either led to believe that if they have not gone into labour by a certain date they will have no option but to accept a repeat caesarean, or that they have a choice between accepting a repeat caesarean or induction, which is often unacceptable to them not only because of the increased risk of rupture, but because it is one of the interventions they are trying to avoid in order to increase their chance of a VBAC, and we must not forget that induction takes the option of a normal birth away from a women.
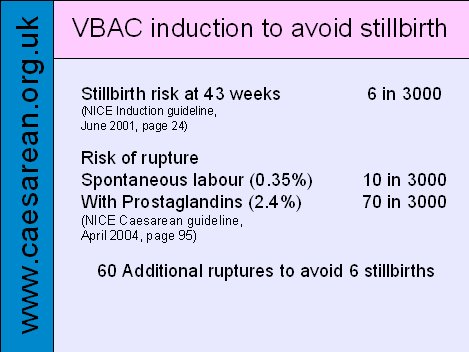
I find the justification for intervention in longer than average VBAC pregnancies hard to understand. Even taking the risk of stillbirth to be as high as 6 in 3000, which is the figure quoted in the NICE Induction Guideline; comparing this to the risk of rupture rising from 0.35% (10 in 3000) to 2.4% (70 in 3000) with prostaglandin induction, figures from the NICE Caesarean guideline - gives a rough estimate that seems to imply that such action would be causing 60 extra ruptures to save 6 stillborn babies. Not a balance of risk that most VBAC women would find favourable. A similar balance of risks and benefit needs to be thought about when considering other forms of induction and repeat caesareans. What are the risks of the repeat caesarean that is being offered, including the risk to the woman and any future babies in other pregnancies that may follow. Can you be sure that you are not leading women to jump from the frying pan into the fire?
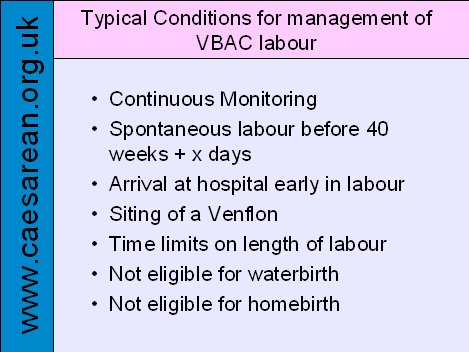
I am not going to go through the other interventions listed here in detail, but as far as I am aware there is no evidence that any of these restrictions improve outcomes in VBAC labours, although I accept there may be good reasons for concerns. However, honesty about why you are offering an intervention, and how limited the evidence is about its effectiveness is crucial to obtaining informed consent. Currently far too many VBAC women are being forced to accept interventions and restrictions without good supporting evidence and without giving consent. Having a scar on your uterus does not take away your right to autonomy, but it should mean that your concerns about the next birth are discussed sensitively and constructively.
All women need support to explore their hopes and fears of the next birth, but this can be even more crucial for a woman who has previously had a caesarean birth, she needs understanding and some resolution of feelings about the previous birth. She needs someone she can discuss her options with; but for many women their interactions with midwives are a series of battles to get their needs met, and to get agreement that their wishes will be respected. This is often a stressful process that has to be repeated with a stream of different people due to lack of continuity of carer.
We desperately need health professionals, and particularly midwives, to listen to women's needs, to remember that women's autonomy should be respected, that the women are the decision makers and the health professional's job is to guide women as to how the service can best accommodate her needs.
So can I bring you back to my initial request that you thought about what information you would give a woman who has had a previous caesarean and is pregnant again. What would you want to know about her previous birth and how would that impact on your discussions.
In the light of what I have said about the rights and the need of women considering VBAC do you feel that you may now be able to address her needs better?
Do you feel that there are constraints within the system that you work that make it difficult for you to properly address the needs of these women? If so what can you and your colleagues do about them?
I would like to just briefly come back to my own personal story. My third child was also born by caesarean, but my fourth child was born at home, another 43 weeks pregnancy (which seems to be normal for me); his birth was healing for me, and for the rest of the family.
Please do not lose sight of the importance of a birth to the psychological health of whole families.
Presentation given at Primary Care 2007 by Debbie Chippington Derrick; Friday 11th May 2007