My own introduction to caesarean section was sudden with the birth of my own daughter. Since then I have been supporting other women, some who are making decisions about a caesarean birth, some that are coping with recovery from a caesarean and others that are looking at their options for a birth following a caesarean. It is nearly a decade since I took on this role along with my colleague Gina Lowdon, nationally for the NCT; which has also meant providing information and support not only directly to mothers, but to others who are informing and supporting them.
My viewpoint is one that has been achieved through the experiences of thousands of women, who have spoken or written to us about their experiences, concerns, fears, and joys of caesarean birth. We encounter a very wide spectrum of views, from women wanting an elective caesarean section without an accepted medical reason to women choosing to give birth at home after several previous caesarean sections.
One of the issues that I wish to focus on is decision making, as acknowledged in the guideline the reason for offering information is to enable informed decision making.
How important is an informed decision? Actually it is a huge part of most of our lives. We live in a society where we expect be able to make our own decisions within an accepted framework. Most of us do not expect to be told what is best for us.
However, how much control a person will want over a decision will vary enormously, some will decide to hand over control to someone they trust and feel is better able to make the decision. (We all do it to some extent - be it only with something such as a financial investment, letting some else cook a meal for us, it is an informed decision in it's own right.) Others will need to maintain full control or even have already made a decision.
Peoples' perceptions of risks and the importance attached to them vary. Many of the recommendations are worded as offering a CS or other intervention, treatment or option. This means a decision about whether to accept or decline the offer is required.

For example the guideline recommends offering a planned CS in a variety of situations, With severe placenta praevia the decision to accept the offer is likely to be readily accepted, even if it is with regret or sorrow, as the risk will considered unacceptable, knowing that she would probably lose her baby and possibly her own life should she refuse the offer.
However in other cases the risks are not nearly as large and more women will feel that they wish to decline the offer. For example, if a woman is offered a caesarean because her baby is breech and declines, then she is still more likely to have a perfectly health baby and avoid surgery than not. In fact the research indicates that she has a 95% chance of her baby being alright, compared to 98.4% if she accepts the caesarean. So her evaluation of how the other risks and inconveniences of caesarean section compare will be important. She may also feel that there are actions that she can take that will reduce the risk to a level below that indicated by the research, many factor can influence the progress of a labour and birth.
This brings me to the next issue that I believe is going to be crucial in the effective implementation of these guidelines. When a woman considers declining the offer of a caesarean, she needs to know her decision will be respected and not undermined. She also needs to know she will be provided with good care that minimises the risks to the baby. Considering breech again, but it would apply to many other situations too, the mother needs to know that the person who is to care for her while she gives birth to her breech baby is both competent and confident in doing so. Without that support for the "alternative choice" an informed decision is not possible. Often I hear women tell me that their hospital "does not do" twin or breech births, they are all by caesarean. Women in these places are not in a position to make an informed decision. We know of many who have been sure that a vaginal delivery with good support would be right for them but have felt forced into surgery, which they consented to because they felt there was no "safe" alternative.
In this case it may be the choice of the lower risk option that feel unavailable to a women. Staff shortages and normal expectations can leave women feeling that hospital is really only their only choice. For other women even if home birth was easily accessible, the norm in the area, they would feel, despite the additional risks, that hospital was still the right place for them to have their baby; but in this case these women would be able to make a real informed choice about where to have their baby.

Again there are going to be perceptions of risks that will mean different women will evaluate the same situation in very different ways.
With ECV - Some women feel very strongly that to try to turn there baby would be wrong, others feel scared by it, but would be willing to try if they felt they could easily back out at any point. Others will be very keen. How important is turning the baby, for the each woman, will play a part. However, how available the service is, along with how experienced the practitioners are will also be relevant.
With continuous support there will be differences in the underlying feelings of women and those who might be available to support the;, but also how welcome additional supporters are on a labour ward, how big the room is or what furniture it contains are likely to have effects too.
With induction after 41 weeks,a family history of babies being born well beyond this is likely to instil greater confidence that this is just a normal variation of pregnancy and change the mother perception of the risk if not the risk itself. The way that a mother is monitored in the days beyond 41 weeks, should she decline the induction, will also affect greatly her decision.
There is more guidance on VBAC
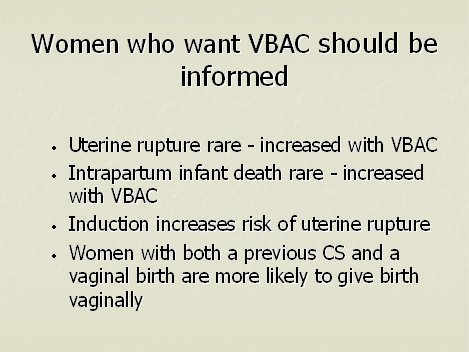
I wish to use as an example a group of women who I have worked with extensively - VBAC women. Many of these women approach us already knowing they either want a VBAC or a repeat caesarean and others are looking for information to help them make the decision.
Their decision is likely to be coloured hugely by their previous experiences and their evaluation of those experiences. It is not uncommon for women not to be prepared to repeat certain parts of the previous experience. However, I am aware that large numbers of these women are adamant that they can change the risks involved and I think that is well accepted for some aspect, but not others. It is not that long ago that the idea that induction may be increasing the rupture rate was not accepted as a real problem, but the research has now shown that it does. Homebirth has been shown to reduce the caesarean rate, and so has intermittent monitoring, rather that EFM. VBAC women can often find themselves "allowed" to labour but under pressure to accept a list of conditions, often conditions that the individual find unacceptable and that many feel contributed to their first caesarean. Facilitating VBAC a full informed decision means opening up vaginal birth with all its possibilities to these women. Yes, they should be offered continuous monitoring and the additional risk of them encountering problems over and above any other women labouring should be explained, but then the women need to be positively supported whether she accepts or declines the offer.
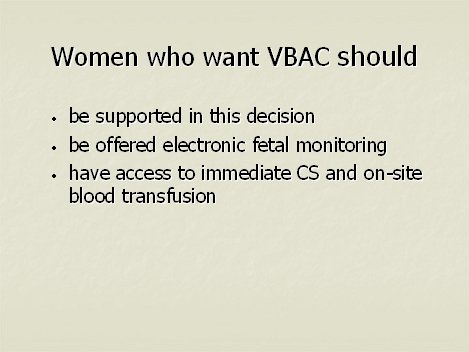
Many women are very sure that if they can get the right environment and level of support, often feeling they need someone they already have a relationship with then they can reduce their risk of encountering problems. Reducing their levels of anxiety and freeing their to labour better. There are several women who have achieved a VBAC after three caesareans over the last decade, there has been agreement the VBAC was only possible in the right environment, with the right support and a trust in their body's ability to birth their baby. There has been a common feeling that the failure to give birth previously was lack of support for them to focus on just giving birth.
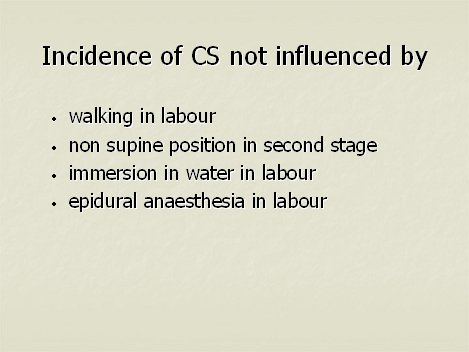
The guideline recommends informing women that these things do not effect the CS rate; but how you feel about something, how secure it makes you feel, how it affects your level of tension are all important and this in turn is for each individual to include in their own evaluation of whether it might effect their personal ability to labour.
Let me use a travel example again - if you are about to make a journey by car and are fearful of the route, including busy roads that you find difficult or a mountain pass that sets off your fear of heights - not only is your perception of the risk changed, but your fear itself may make you more likely to have an accident.
So consider the same for the birth process, which is chemically affected by stress hormones. How much greater might these effects be in changing the risk for different individuals. We must remember that the measure of risk can only ever give us a guide for the population as a whole and in each individual case the relevance of the information needs to be assessed afresh.
Many of the recommendations will be of little interest to most women, although some will benefit from increased accessibility of this information. However there are that are likely to get attention from more women; again there will be issues of perception, varying circumstances and availability of support and acceptance by health professional of a woman's rejection of the offer.
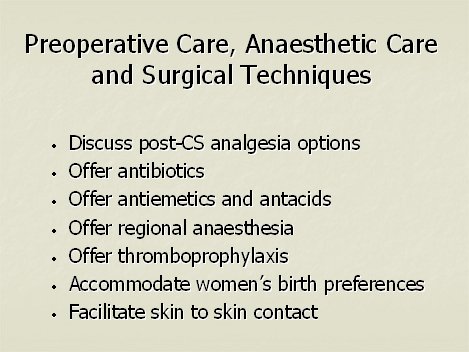
In the case of many of these even if women usually are happy to take the advice of their health professionals, more women will have a better understanding of and involvement in what happens to them during a CS; for example at present many women can be unaware that they have been given any drugs, other than those for the regional anaesthesia.
Again there will be considerable difference in the importance of these things for different women, but again there will be different abilities to make an informed choice depending on the support that is provided to the women. Many caesarean women complain that the food is served a distance away from the ward they are on and their reduced mobility makes it difficult to walk that far; in order not to continue preventing women from eating post caesarean, the accessibility of meals needs to be addressed. When making a decision about returning home early, individual circumstances and feelings will affect the decision, but also the availability of midwifery care in the community will also be important, in facilitating informed choice.
Presentation given at the launch of the NICE Caesarean Guideline by Debbie Chippington Derrick; 29th April 2004 RCOG, London